George L. Bakris, M.D1., Marshall Dickholtz, Sr., D.C2., Peter Meyer, Ph.D. 1, Glenda Kravitz, M.S. 1, Elizabeth Avery, MS1, Martha Miller BA3, Charles Woodfield, R.Ph., D.C.3, Jonathan Brown, D.C.2, Bruce M. Bell, M.D. 3 1-Rush University Hypertension Center, Chicago, IL. 2-Dickholtz Chiropractic Center , Chicago, IL, 3-Office of Bruce Bell, Fox River Grove, IL
ABSTRACT
Anatomical abnormalities of the cervical spine at the level of the Atlas vertebra are associated with relative ischemia of the brainstem circulation and increased blood pressure (BP). Manual correction of this malalignment has been associated with reduced arterial pressure. This pilot study tests the hypothesis that correcting malalignment of the Atlas vertebra reduces and maintains lowering BP. Fifty drug naïve (n=26) or washed out (n=24) subjects with Stage 1 hypertension were evaluated using a randomized, double blind, placebo-controlled study design at a single center. Subjects received no antihypertensive meds during the eight-week study duration. After baseline measures subjects were randomized to receive a National Upper Cervical Chiropractic (NUCCA) procedure or a sham procedure. Statistical analysis was performed comparing baseline and week 8 visits. The study was designed with 90% power to detect an 8/5 mmHg reduction difference in arterial pressure at eight weeks over the placebo group. The study cohort consisted of 70% males, 2% Hispanic; mean age 52.7+9.6 years. There were no major differences in baseline demographics found between the two treatment groups. The primary results of the study are noted in the Table. No adverse effects were recorded. We conclude that restoration of Atlas alignment is associated with marked reductions in blood pressure similar to the use of two-drug combination therapy. Larger studies are needed to validate these findings
|
NUCCA (N=25) |
PLACEBO (N=25) |
|||
|
Baseline |
Visit 8 |
Baseline |
Visit 8 |
|
| Systolic BP (mmHg) |
147+ 6 |
130+ 10* |
145+6 |
142+11 |
| Diastolic BP (mmHg) |
92+ 8 |
82+ 9* |
91+8 |
89+ 9 |
| Lat. Displacement ofSpinal Column (C7) (0) |
1.0 |
0.04# |
0.6 |
0.5
|
*After adjustment for baseline levels, the treatment effect for Systolic BP was significant at the 0.0001 level and Diastolic BP at the 0.002 level. #After adjustment for baseline values, treatment effect for Lateral Displacement of spinal column at C-7 was significant at the 0.002 level.
BACKGROUND
- Studies note that arterial compression of the left lateral medulla oblongata by looping arteries of the base of the brain in 51 of 53 hypertensive patients undergoing left retromastoid craniotomy and microvascular decompression for unrelated cranial nerve dysfunctions; 76% of these individuals had marked lowering of blood pressure following surgery. Such compression was not noted in normotensive patients.1
- Studies to clarify the mechanism by which decompression of the left rostral ventrolateral medulla alleviate neurogenic hypertension have been performed. They indicate that a sub-population of hypertensive patients have amelioration of their hypertension after microvascular decompression. Changes in the anatomical position of the Atlas vertebra and subsequent changes in the circulation of the vertebral artery lends itself to worsening of hypertension.2,3
- Recent studies using MR imaging evaluated the relationships between the upper ventrolateral medulla and vertebral arteries and branches in normotensives and controls. They note compression in 90.6% of the 32 hypertensive patients, in contrast to controls and those with secondary hypertension.4
- Two other studies using MR imaging also showed a significant association between compression of the vertebral artery and changes in the posterior fossa of hypertensive but normotensive individuals.4,5
PURPOSE OF STUDY
This pilot study examines the relationship between nonsurgical interventions to align the Atlas vertebra and changes in blood pressure and heart rate.
HYPOTHESIS
Those with hypertension and absence of neck pain will have misalignment of their Atlas vertebra where upon correction will lead to significant lowering of their blood pressure.
METHODS
Study Design – randomized, double-blind, with a placebo control. The trial was conducted in accordance with the Good Clinical Practice/ International Conference on Harmonization guidelines, with mandatory signed informed consent by the Institutional Review Board.
Exclusion Criteria
- No physical evidence of Atlas misalignment on preliminary screening
- Stage-2 or higher hypertension
- Prescribed regimens of more than two (2) antihypertensive medications
- Incapacity/unwillingness to suspend antihypertensive regimens for screening/study duration
- Second- or third-degree heart block without pacemaker
- Concomitant refractory angina pectoris
- Recent (<12 months) stroke, MI, or cardiovascular surgery
- BMI >39
- Active drug/alcohol addiction (or abstinent <1 year)
- Psychiatric diagnosis
- History of cervical fractures or cervical surgeries
- History of prior Atlas alignment by National Upper Cervical Chiropractic Association (NUCCA) protocols
- Unwillingness to forego other chiropractic/osteopathic services for study duration;
First Visit Atlas Assessment
- Supine leg-length check: a misaligned Atlas results in leg-length disparities, apparent in comparisons of heel positions when patient lies in a supine position; when the patient is instructed to turn his/her head to the left or right, the heel position disparity changes. (Heels that appear parallel to one another, or that remain static on head-turning, signal that the Atlas is not misaligned.)
- Paracervical skin temp
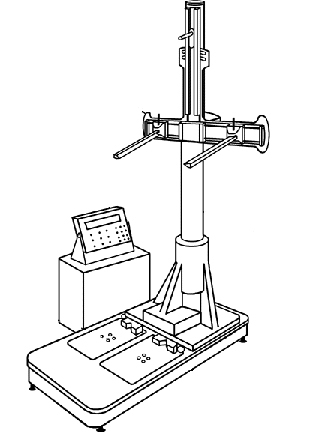
- Postural analysis: using an “Anatometer,” (see figure) provides pertinent diagnostic details of postural asymmetries.
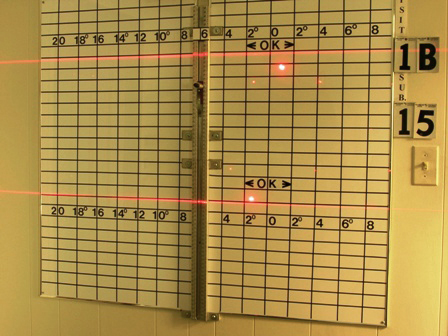
- Lateral spinal column displacement at C-7 or T-1, also measuring Atlas misalignment’s typical “head-tilt”;
- Weight-bearing inequalities, Left versus Right, as calibrated by a pair of weight-sensitive platforms (electronic scales) coupled to transducers, with values reported in digital read-outs, of the portion of total body weight supported by each foot.
- Pre-Alignment Craniocervical Radiographs: Three x-ray views to measure and visualize (in three dimensions) the Atlas misalignment’s precise degree and orientation, specifically: a) Lateral C-Spine (to pinpoint Atlas’ sagittal position, for best visualization of its posterior-arch attachments, Atlas position’s most reliable landmarks), to inform optimal central-ray direction/angle for the Nasium view); b) Nasium, front-on AP skull view, with central ray aimed toward the infra-orbital meatal line; c) Vertex, through the crown of the skull and into the neural canal
Intervention Group
- Patient is positioned on a low (8-inch) side-posture table, depending on misalignment’s orientation), with head precisely placed on a curved, mastoid support, which serves as
the intervention’s “fulcrum.” Several measurements inform clinician’s optimum body stance and vectors relative to the patient.
- For precision, support and control, the clinician firmly clasps the non-dominant hand around the dominant wrist, and then precisely positions the dominant hand’s pisiform on the appropriate “corner” of the Atlas transverse process to use it as the intervention’s “adjustment lever.”
- A series of precise, subtle, external nudges causes Atlas to recoil into normalized alignment, reseating occipital condyles into Atlas’ lateral masses.
Control Group
Sham intervention was designed to be indistinguishable to the patient from an authentic alignment, possible only because of the delicacy of the procedure. This group’s intervention were identical to those employed for the Treatment Group except the clinician intentionally and slightly misplaced the patient’s head on the (“fulcrum”) support device and misplaced his hands, intentionally to miss the Atlas’ lateral-mass contact point for the crucial “lever nudge.”
Post Intervention Assessment
Repeat measurements of all of the aforementioned variables. To support blindedness, sham “realignments” and assessment protocols were scheduled for members of the Control Group. Some 85% of Treatment Group Patients required only one (1) intervention (remained “in Atlas alignment”) during (8)-visit, (roughly) two month course of the trial.
Anatomer
Provides Left and Right weight-bearing scales and other calibration mechanisms designed to provide clinical measures of Atlas misalignment.
Main measures include: 1) degree of pelvic distortions in the frontal and transverse planes; 2) pelvic distortions in the horizontal plane, indicated by unequal distances (Left versus Right) between the iliac crests and the soles of the feet;
STATISTICS
The study was designed to have 90% power for detecting a difference of 10 mmHg in SBP change between the treatment and control groups with 25 patients per group, anticipating a 10 % dropout rate.
Demographic and baseline characteristics were compared using t-tests, Pearson’s chi-squared tests and Fisher Exact tests as appropriate. The primary analyses used t-tests to compare the change in blood pressure from baseline to week 8 between the two groups.
Secondary analyses used regression techniques to adjust for baseline level. All tests were two-sided and p-values less than 0.05 were considered significant. Paired t-tests were used to determine if change from baseline to 8 weeks was significant within groups.
Pre- to post-adjustment values at baseline within each group to ensure that treatment had been effective in the treatment group and that no significant difference in condition occurred in the control group. We also compared post-adjustment at baseline to the 8 week measure. Baseline comparisons in the control group were important both in terms of establishing no treatment effect as well as verifying that no harm was done by the sham adjustment. Comparisons of baseline to 8 weeks were important in the treatment group to verify persistence while they were important in the control group to ensure no spontaneous adjustment might explain a potential lack of difference in the two groups.
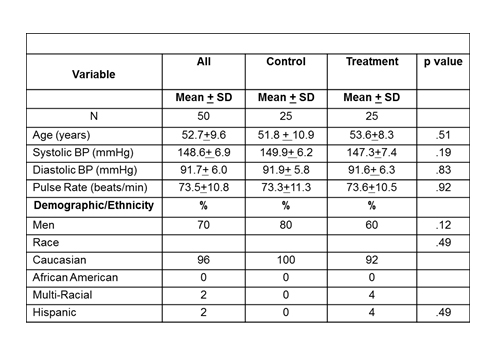
Baseline Descriptive Characteristics
X-ray Measures of Atlas Position
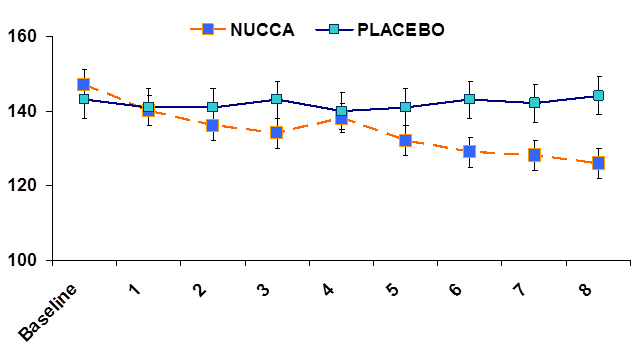
Trends in Systolic Blood Pressure in Both Groups over the Eight Week Period
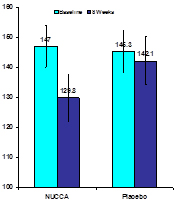
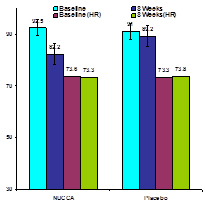
Changes in Blood Pressure (mmHg) and Heart Rate
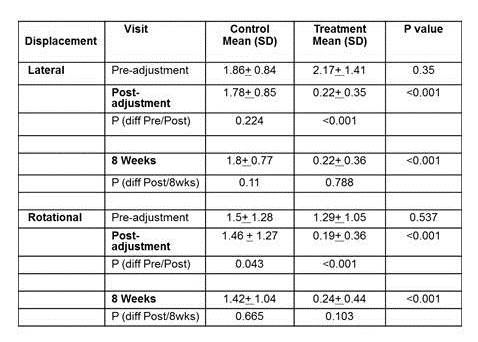
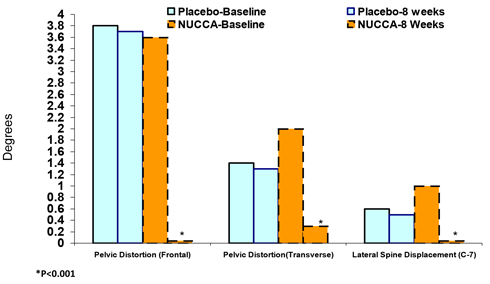
Change in Alignment Variables
SUMMARY AND CONCLUSIONS
This pilot study shows that correction of misalignment of the Atlas vertebra lowers and sustains reductions in blood pressure for at least 8 weeks in people with Stage 1 hypertension.
Individuals with Stage 1 hypertension who have no apparent etiology and lack a family history (42% of our group lacked family history of hypertension) may have cervical neck abnormalities related to the Atlas Vertebra.
Further studies need to be done to assess the mechanisms related to this treatment and confirm the effect as it may provide a partial benefit in the treatment of hypertension
REFERENCES
- Jannetta PJ, Segal R, Wolfson SK, Jr. Neurogenic hypertension: etiology and surgical treatment. I. Observations in 53 patients. Ann Surg 1985; 201(3):391-398.
- Reis DJ, Ruggiero DA, Morrison SF. The C1 area of the rostral ventrolateral medulla oblongata. A critical brainstem region for control of resting and reflex integration of arterial pressure. Am J Hypertens. 1989 Dec; 2(12 Pt 2):363S-374S.
- Akimura T, Furutani Y, Jimi Y, Saito K, Kashiwagi S, Kato S et al. Essential hypertension and neurovascular compression at the ventrolateral medulla oblongata: MR evaluation. AJNR Am J Neuroradiol 1995; 16(2):401-405.
- Coffee RE, Nicholas JS, Egan BM, Rumboldt Z, D’Agostino S, Patel SJ. Arterial compression of the retro-olivary sulcus of the medulla in essential hypertension: a multivariate analysis. J Hypertens 2005; 23(11):2027-2031.
- Nicholas JS, D’Agostino SJ, Patel SJ. Arterial compression of the retro-olivary sulcus of the ventrolateral medulla in essential hypertension and diabetes. Hypertension 2005; 46(4):982-985.